Autoimmune Diseases and Your Oral Health
How autoimmune diseases affect oral health
Your immune system defends your body from harmful bacteria and viruses, but in autoimmune diseases, a disruption in your immune system can cause it to attack your own tissue. Millions of Americans suffer from autoimmune diseases, a broad category of diseases which can manifest themselves in many different ways.
There are more than 80 different autoimmune diseases, ranging from nearly asymptomatic disorders to severe diseases that require regular medical attention. Every autoimmune disease has a unique set of symptoms, and it can affect nearly every part of your body — including your mouth and your teeth.
Autoimmune conditions can either start at birth or develop later in life. Scientists have identified many factors that could play a role in causing autoimmune diseases, including genetics and hormone levels. You should always be aware of symptoms like lightheadedness, fever, and unusual fatigue that could indicate an autoimmune condition.
Tip: Oral health problems can often be a symptom of an autoimmune disease. Here are common autoimmune conditions that can affect your oral health, and the symptoms to look out for.
Sjögren’s syndrome
Sjögren’s syndrome is a common autoimmune disease that mostly affects middle-aged and older women. It impacts your liquid-producing glands, including your tear ducts, tissue glands, and salivary glands. Because Sjögren’s can reduce saliva production, it can lead to dry mouth, trouble swallowing, and cavities. It can also increase your risk of developing an oral infection.
Crohn’s disease
People with Crohn’s disease usually begin to show symptoms early in life, when they are in their thirties or younger. Although the most common manifestation is swelling and irritation of the gastrointestinal tract, it can also cause swelling and infection in your gums and lips.
Diabetes
Type 1 diabetes is a result of your immune system limiting insulin in your pancreas. When left untreated, it can lead to reduced blood supply throughout your body — including your gums. This makes your gums more likely to become infected, sore, and ulcerous. Type 2 diabetes can lead to similar oral infections.
Periodontal disease: autoimmune or not?
Scientists haven’t determined the exact cause of periodontal disease (also called periodontitis), which can lead to gum inflammation, oral infections, and tooth loss. In many ways, periodontitis resembles common autoimmune diseases. Vulnerability to periodontitis runs in families, and it shares many oral symptoms with autoimmune diseases like Sjögren’s syndrome and type 1 diabetes.
Some studies suggest that periodontitis may be an autoimmune disease, while others believe it simply has an autoimmune component. Regardless of its origins, if you are showing symptoms of periodontitis, you should visit a dentist as soon as possible.
Schedule regular dental appointments
One common trait shared by autoimmune diseases is that they are chronic. Although modern medicine has led to successful treatment options for many autoimmune diseases, these conditions will continue to exist in your body throughout your life.
If you suffer from chronic oral health problems, no matter the cause, you should maintain a regular dental health routine and schedule regular appointments with your dentist.
Schedule an appointment with Espire Dental today!

Stop putting off your smile
Book your visit now—it’s easier than you think
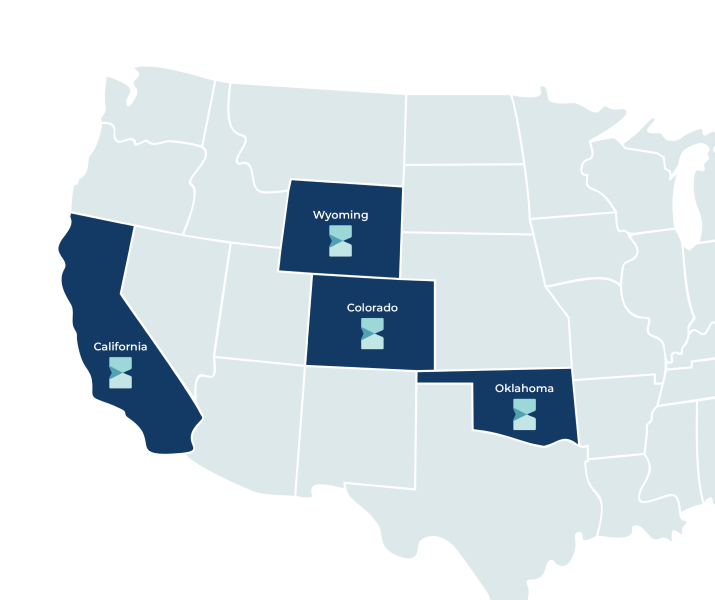
Find your Espire location